Parkinson's Disease
Parkinson’s disease is a progressive neurodegenerative disorder that primarily affects the movement system and has significant implications for patients and their families. While medication is the first line of treatment, neurological rehabilitation approaches alongside drug treatments play a crucial role in alleviating patient symptoms.
We employ technological approaches to assist with symptoms such as uncontrollable shaking, balance and coordination difficulties, and stiffness.
Our rehabilitation aims to maintain the highest possible quality of life for the longest possible time, depending on the neurological impact of Parkinson’s disease on the individual.
The goals of our rehabilitation treatment include:
- Enhancing muscle and joint flexibility
- Improving mobility, strength, and range of motion
- Correcting body posture during walking
- Maintaining and improving step length during walking
In addition to addressing motor system issues, our rehabilitation process also targets cognitive functions, sleep disorders, and autonomic and sensory dysfunctions. We tailor a personalized training program to each patient’s condition.
Our comprehensive approach includes:
Parkinson’s Disease Rehabilitation
Early diagnosis of Parkinson’s disease is crucial. While early treatment may not completely prevent symptoms, it can delay the onset of severe symptoms for years. Rehabilitation is vital for many Parkinson’s patients, particularly following new treatments such as deep brain stimulation. It helps patients return to their normal lives under optimal conditions and is also essential for those with advanced Parkinson’s disease experiencing balance or gait disorders.
A sustained, holistic treatment approach—including medication, deep brain stimulation, movement therapy, cognitive training, and speech therapy—is key to slowing the progression of symptoms.
Our holistic approach ensures the best medical treatment combined with intensive daily therapies. Your daily treatment program is tailored to your current condition and goals, with up to 4-6 personalized therapy sessions per day.
We utilize advanced technological approaches to assist patients with unwanted movements, balance and coordination difficulties, gait disturbances, and stiffness:
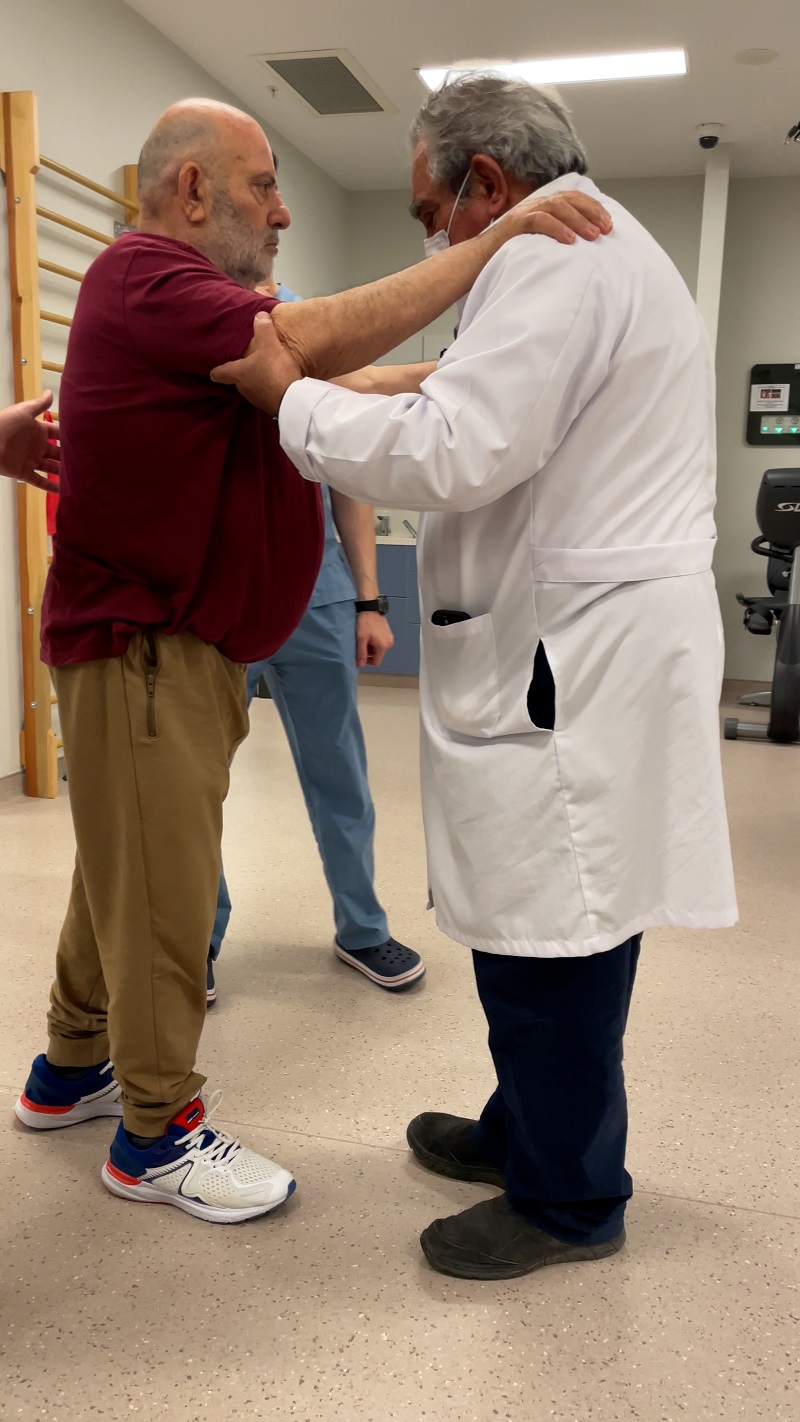
- Physiotherapy: Conventional exercises improve muscle strength, coordination, and mobility.
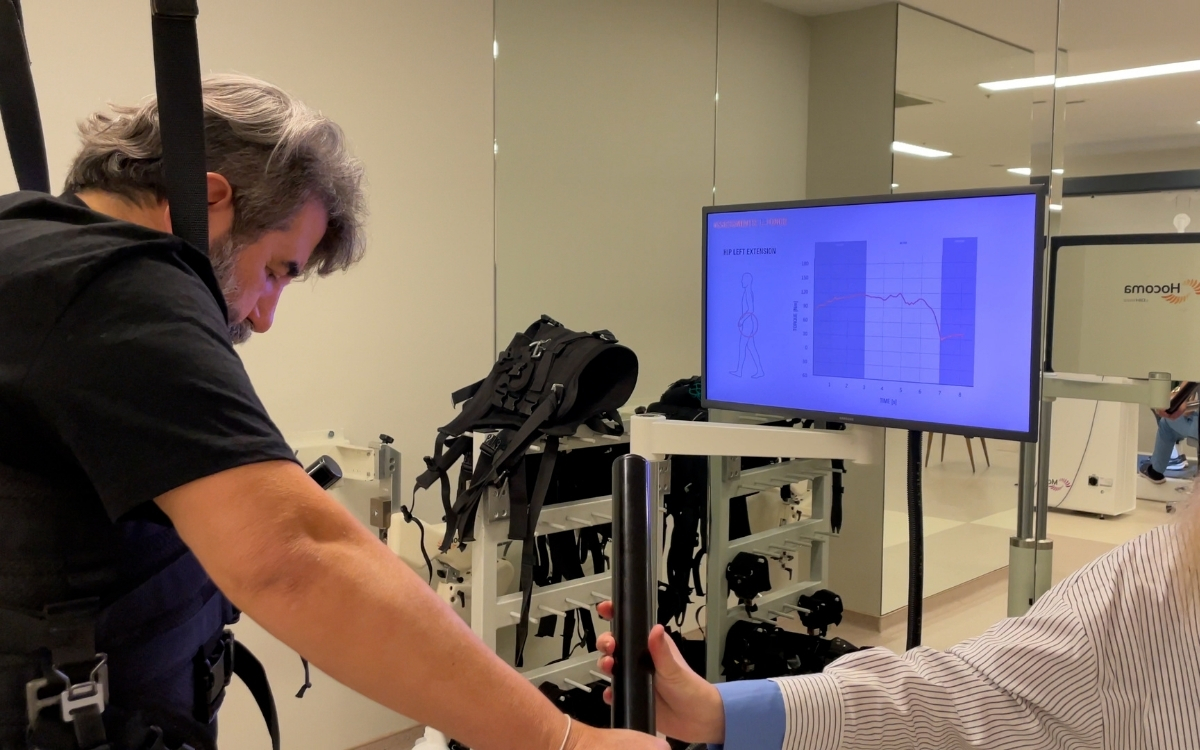
- Robot-Assisted Walking Training: This technology helps both adults and children regain walking abilities and leg functions more quickly and accurately than traditional physical therapy.
- Robotic Hand-Finger-Arm Training: Robotic devices support and strengthen the patient’s arm, aiding the brain’s re-learning process through intensive, repetitive treatment.
- Virtual Reality-Assisted Gait and Balance Training: A virtual reality environment offers a range of exercises to improve balance, walking, and cognitive function.
- Electrical Stimulation: Used to prevent muscle wasting and to strengthen muscles.
- Occupational Therapy (Ergotherapy): Enhances sensory and motor development to improve daily living activities, such as dressing, feeding, brushing teeth, meal preparation, and housework.
- Cognitive Therapy: Aims to improve cognitive abilities such as memory, processing, problem-solving, social skills, judgment, and safety awareness.
- Speech Therapy: Focuses on restoring lost abilities in speaking, listening, writing, and understanding.
- Respiratory Therapy: Helps clear obstructions in the respiratory tract and supports physical activity and effort.
Frequently Asked Questions
Parkinson’s disease is one of the most common neurodegenerative disorders that affects the central nervous system. It is characterized by tremors, bradykinesia (slow movement), rigidity, and balance issues. Approximately 10 million people worldwide are affected by Parkinson’s disease. While the exact causes remain largely unknown, the disease is associated with the progressive decline and degeneration of brain cells responsible for dopamine production. Men are more frequently affected than women, and the disease typically manifests between the ages of 50 and 60. Parkinson’s disease impacts various brain functions, including speech, movement, and cognitive abilities.
Erkekler kadınlardan daha sık etkilenir ve hastalık genellikle 50 ila 60 yaşları arasında ortaya çıkar.
Parkinson hastalığı konuşma, hareket veya bilişsel yetenekler gibi bir veya daha fazla beyin fonksiyonunu etkiler.
The symptoms of Parkinson’s disease are multifaceted and can vary widely among individuals, particularly as the disease progresses. Symptoms are generally mild in the early stages but tend to become more pronounced over time.
Typical physical symptoms of Parkinson’s disease include:
- Tremors (resting tremors)
- Muscle stiffness (rigidity)
- Shuffling gait with small steps
- Reduced arm swing
- Characteristic mask-like face with minimal or no facial expressions
- Balance issues
Typical non-motor symptoms may include:
- Sleep disturbances, such as talking or sleepwalking
- Urinary incontinence
- Depression
- Anxiety
- Dizziness
- Loss of smell
In addition to these symptoms, Parkinson’s disease is often accompanied by sleep disturbances, constipation, bladder issues, and difficulties with swallowing and chewing.
Treatment Stages for Parkinson’s Disease
Treatment for Parkinson’s disease varies based on the severity of the condition and the specific symptoms experienced. Typically, managing Parkinson’s disease involves a multidisciplinary team working collaboratively. This team may include:
- Neurologists
- Neurosurgeons
- Physical therapy and rehabilitation specialists
- Physiotherapists
- Occupational therapists
- Dietitians
- Psychologists
In addition to enhancing the effects of surgical treatments such as medication and deep brain stimulation (DBS), rehabilitation programs are designed to maximize functional ability by promoting activity-related neuroplasticity.
Rehabilitation is crucial for many Parkinson’s patients. It plays a key role after new treatments, such as deep brain stimulation, to help patients return to their daily lives under optimal conditions. Rehabilitation is also essential for those with advanced Parkinson’s disease, particularly for addressing issues such as balance and gait disorders.
Robotic Rehabilitation for Parkinson’s Disease
Robotic rehabilitation for Parkinson’s disease begins with a comprehensive evaluation of the patient’s condition. Before starting treatment, a personalized plan is developed, considering factors such as mobility, balance, coordination, and individual strengths and weaknesses.
The treatment employs robotic devices to enhance mobility, balance, and coordination. For instance, arm and walking robots enable patients to perform various exercises aimed at strengthening their leg and arm muscles. Virtual reality applications simulate the daily challenges faced by Parkinson’s patients, helping them prepare for real-life difficulties.
Throughout the treatment process, the patient’s progress is continuously monitored, and the treatment plan is adjusted as needed. This approach ensures that patients achieve the most effective results during their rehabilitation.
Inpatient Physical Therapy
During inpatient physical therapy, patients collaborate with a multidisciplinary team that includes physiotherapists, occupational therapists, rehabilitation nurses, speech and swallowing therapists, respiratory therapists, psychologists, and dietitians, all under the leadership of a Physical Therapy and Rehabilitation Specialist Physician. This comprehensive care requires 24-hour attention and treatment.
Upon admission to our inpatient facility, patients receive a fully personalized rehabilitation program tailored to their specific needs, with 4-6 hours of treatment daily. The rehabilitation process involves an intensive exercise regimen using robotic rehabilitation devices, holistic consultations, and regular evaluations to track progress.
Key Features:
- 4-6 hours of one-on-one rehabilitation daily
- Multidisciplinary patient care involving all relevant medical specialties
- 24-hour supervision by medical professionals
- Personalized robotic neurorehabilitation program addressing all patient needs
Four Key Factors for Successful Rehabilitation:
- Multidisciplinary Hospital Support:
- Access to a comprehensive range of medical specialties.
- Experienced Rehabilitation Team:
- Skilled physical therapists and rehabilitation professionals.
- Advanced Technological Support:
- Robotic Devices:
- Walking Robot
- Hand Robot
- Arm Robot
- Advanced Walking and Balance Robot
- Technological Innovations:
- Integrated Sensors
- Virtual Reality
- Body Weight Systems
- Touch Screens
- Maximizing Healing Potential:
- Intensive and comprehensive treatment program, typically lasting 4-6 hours per day, designed to stimulate optimal recovery.